Brain-derived neurotrophic factor (BDNF) is a protein, one of a number of nerve growth factors. The longstanding dogma that the brain does not make new nerve and brain cells has been dropped; neurons require BDNF for their survival, and it promotes the growth of new ones. Expression of the BDNF gene is decreased in Alzheimer’s and other neurological disorders. Fasting and exercise increase brain-derived neurotrophic factor.
Lower BDNF levels are associated with depression, and antidepressant treatment raises levels, which suggests that changes in brain neuroplasticity are linked to depression and its treatment. It seems to be the case that brain plasticity must be kept at a normal or basal level, and when it is not, depression could result.
BDNF also appears to be related to memory and cognitive function.
So, BDNF appears to be very important for brain and mental health. It could mean the difference between a healthy old age and dementia. Can we go about raising it, or ensuring that levels remain adequate, and thus prevent cognitive decline or mental illness?
It seems that we can. In rats, calorie restriction (CR) increases both BDNF and the level of neurogenesis. CR does the same in primates.
As we’ve discussed previously, CR is difficult to maintain and is a hard sell for most people. But intermittent fasting has many or even more of the benefits of CR. Maybe fasting can increase BDNF. From Mark Mattson and co-author:
Emerging findings suggest that brain-derived neurotrophic factor (BDNF) serves widespread roles in regulating energy homeostasis by controlling patterns of feeding and physical activity, and by modulating glucose metabolism in peripheral tissues. BDNF mediates the beneficial effects of energetic challenges such as vigorous exercise and fasting on cognition, mood, cardiovascular function, and on peripheral metabolism. By stimulating glucose transport and mitochondrial biogenesis BDNF bolsters cellular bioenergetics and protects neurons against injury and disease. By acting in the brain and periphery, BDNF increases insulin sensitivity and parasympathetic tone. Genetic factors, a ‘couch potato’ lifestyle, and chronic stress impair BDNF signaling, and this may contribute to the pathogenesis of metabolic syndrome. Novel BDNF-focused interventions are being developed for obesity, diabetes, and neurological disorders.
Congruent with the above excerpt, BDNF levels are lower in type 2 diabetes, which is the premier example of the couch-potato lifestyle.
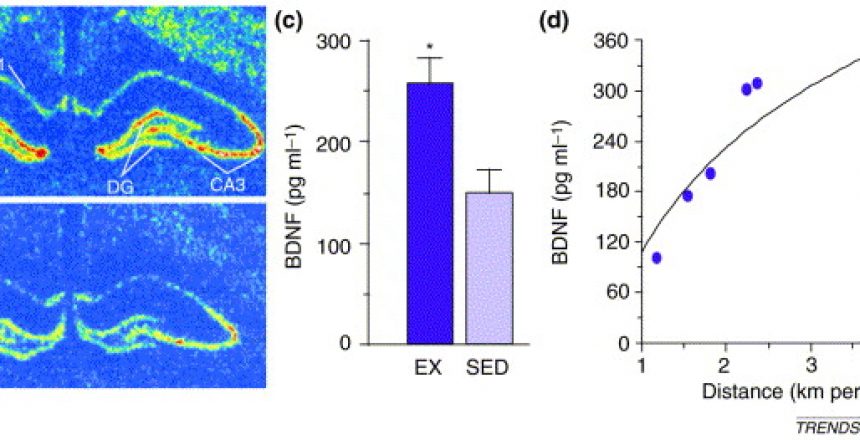
Exercise also increases levels of BDNF, in rats, and in humans, and exercise is known to increase the potential for brain plasticity. Exercise also increases brain volume.
Also well worth mentioning is that zinc supplementation decreases depression and increases BDNF at the same time.
So, the couch-potato lifestyle is associated with, or leads to, lower levels of BDNF, as well as metabolic disorders that are in turn associated with lower BDNF. Intermittent fasting and exercise raise levels of BDNF, increase brain volume, protect against stresses and chemical and physiological insults to the brain, and lead to better cognition, and protect against depression and dementia. The lesson here seems to be that being a couch potato diminishes brain function, and being active and not eating all the time protects and even enhances brain function.
And don’t be zinc deficient either.