Many people, perhaps most, think that cancer is just something that strikes. That there’s little you can do about avoiding it – other than not smoking cigarettes. That is not the case, since there’s a link between insulin and cancer, and we can control insulin levels.
Associations between insulin and cancer
People who are in the highest quintile (fifth) of insulin levels have a 62% higher risk of dying from cancer, and a 161% risk of dying from gastrointestinal cancer. (Perseghin, Gianluca, et al. “Insulin resistance/hyperinsulinemia and cancer mortality: the Cremona study at the 15th year of follow-up.” Acta Diabetologica 49.6 (2012): 421-428. Link)
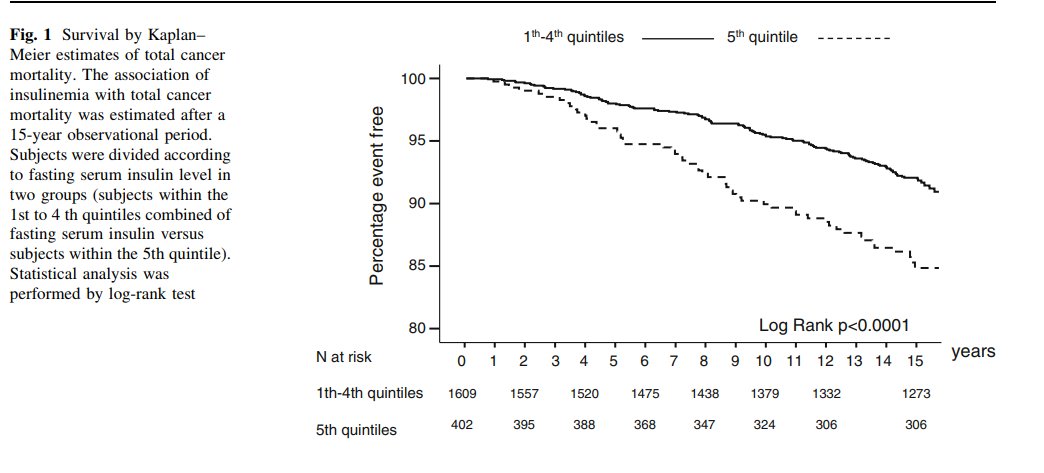
The above chart shows survival in terms of death from cancer in people in the top quintile (fifth) of fasting insulin, vs quintiles 1-4. You’re much more likely to die from cancer if you have high insulin. The association was even worse for GI cancer.
This doesn’t prove that high insulin causes cancer, but it’s quite suggestive. We know that obesity and diabetes are associated with higher cancer risk, and insulin may very well be why.
Diabetics have about double the risk of cancer. (Ref) That’s compared to the rest of the population, most of whom either have metabolic syndrome, are overweight or obese, are skinny fat, and in general likely to have metabolic problems. What’s the risk of cancer compared to people with healthy metabolic control?
Laron dwarfism may provide some clues.
In people with Laron dwarfism or other forms of growth hormone or IGF-1 defects, none of the IGF-1 deficient people had cancer, whereas 9-24% of their relatives had a history of cancer. (Ref) This refers to deficiency of IGF-1, or insulin-like growth factor 1, not insulin itself, but the two are closely related, with a correlation between the two of 0.58 in obese people. (Ref)
Seems at least possible that if no insulin, then no cancer.
Obesity greatly increases the risk of colon cancer, and “insulin resistance and type II diabetes loom large in the theoretical framework that connects obesity and colon cancer.” (Ref)
There’s a 20-fold difference in colon cancer rates between low and high incidence regions. (see above ref.)
All of this evidence points in the direction of higher insulin increasing risk for cancer.
Ideally, we’d like to see an experiment in which lowering insulin, without doing anything else, means less cancer.
Experimentally lowering insulin
Such an experiment has now been done, in mice, for the first time. (Endogenous insulin contributes to pancreatic cancer development Anni MY Zhang, et al. bioRxiv 530097; Link)
Mice were genetically engineered to have lower insulin, and they had 50% fewer precancerous lesions in the pancreas. This is highly suggestive. Makes sense too, since insulin is a growth factor and cancer is runaway growth.
“Collectively, our data indicate that endogenous insulin hypersecretion contributes causally to pancreatic cancer development. This suggests a modest reduction in fasting insulin via lifestyle interventions or therapeutics may be useful in cancer prevention.”
Cancer cells require insulin, and they have a high density of insulin receptors, so they can get all their primary fuel, glucose, from the blood.
A high insulin and high cancer environment – ours
We live in a high insulin environment. Food that’s loaded with sugar and refined grains is everywhere, and in abundance.
More than 70% of Americans are overweight or obese, which means many of them have high insulin.
Being sedentary also means higher insulin. Exercise lowers insulin resistance, which translates to lower insulin.
So, to lower your cancer risk overnight, lead a low insulin lifestyle.
You do that by avoiding ultra-processed foods, by exercising, and by practicing intermittent fasting.
And of course, getting or staying lean and muscular. (Although normal body fat and muscle percentage are different for women, the same applies to them too.)







20 Comments
I believe insulin is also part of mTOR signalling, so chronically high insulin equals chronically high mTOR instead of pulsed mTOR. I believe there is also some evidence that lack of insulin pulses may create issues as well, partially due to reduced signalling for things that are desirable in pulses (like mTOR) but I haven’t looked at that recently.
Also, I believe chronically high insulin provokes unnecessary inflammation which is in itself cancer-promoting. Many studies on this tend to be deceptive however since they combine insulin and blood-sugar, and in doing so claim that insulin is anti-inflammatory.
IIRC, one of the main differences between a normal cell and a cancer cell is that cancer cells have forgotten how to oxidize, and can only obtain energy by fermentation (of sugars).
Thus, no sugar = no fuel for cancer cells
And of course no sugar = no insulin response
So if true, low/no insulin is not a cause of low/no cancer, but both are instead results of low/no sugar. FWIW
That is more or less the case. Since cancer cells need glucose for anaerobic glycolysis, as you say, they have a high need for insulin also and have high insulin receptor density. If there’s enough insulin around, a cancer cell can always get enough glucose. The reason why low carb diets may be effective against cancer is not by lowering glucose, but lowering insulin.
Mr. Mangan,
So insulin (and thus carbs) is bad but so is protein (above what you need to maintain reasonable muscle mass which isn’t much) so all that is left to eat is fat (with a little protein and a small amount of carbs from green veggies).
This is pretty much what Dr Rosendale recommends (he is a diet guru so don’t know if his findings are legitimate).
Just a note: when I eat very low carb my lifts go way down – even with low volume lifting. I simply can’t get the intensity to deadlift, bench, pistol squat, etc nearly as well. Other people I know have found the same thing.
I don’t believe you’re eating enough meat. My PRs have increased since dropping to basically zero carb and body fat has decreased noticeably in a short time.
Google: Vince Gironda
Could be. There are some recent studies that show that most people can only use about .25 g/kg-BW/meal of protein for synthesizing new muscle and that even extreme outliers can only use about .4 g/kg. That’s only 17-28 g of protein per meal for me so that’s approximately what I eat which means 3 or 4 ounces of meat per meal. I am thinking of Mangan’s post on too much protein and life-extension. My goal is to live long and age well so I can see my great grandchildren.
However, can’t excess protein be turned into glucose? So I wonder if the effect you’re seeing from eating additional meat is just the same as adding more carbs – you get more glucose and thus, more glycogen stores?
I will google him. Thanks for the info.
Bruce, studies showing limited use of protein were done using fast proteins like whey. To my knowledge, there aren’t any that show that protein from whole foods acts in this way. Excess protein, however that’s defined, isn’t turned into glucose; gluconeogenesis is a demand-driven process.
Also, I’ve changed my thinking quite a bit on the issue of protein and life extension. As far as I can see, carbohydrates activate insulin, IGF-1, and mTOR far more strongly than protein and are therefore the major threat to life extension in the diet.
Mr. Mangan,
Yes, I have also read that the “how much protein” studies involved isolated proteins, usually either whey or egg. The authors of the studies seem to suggest that a little more protein may be required (since the rise in amino acid levels in the bloodstream is slowed/blunted) for mixed meals but they never really quantify it. Someone needs to study this.
The Okinowan diet seems to be a life-extending diet but no one seems to agree how much protein they eat. Some sources claim they eat very little animal protein. Other sources seem to suggest they eat a pretty fair amount. They don’t eat a lot of calories, and a good portion of their diet is starchy tubers. They are not large people but some of that may be genetics.
Has your assessment of calorie restriction for life extension changed?
Thing about Okinawans and other Blue Zones, is there’s so much going on besides diet: sun, physical activity, social connection and family, religion. Blue Zones. I haven’t changed my mind about CR and longevity.
I have wondered about the fasting thing – whether your body can use more protein than usual after a long fast. Or maybe it’s just that your body conserves protein in a fast as Fung and Rosendale have suggested.
I suspect we may have different goals – you might be a serious weightlifter/bodybuilder whereas I just want to age reasonably well.
There is no way the body can only use .25g/kg of protein for MS. Just google the likes of Shawn Baker, Ted Naiman, Martin Berkhan etc some of whom only eat twice/ day. I agree with your points Dennis. At least 40g of protein per meal in 2 or 3 meals for big Mtor pulses and daily 16-18 hour fast for ampk boost (autophagy). Less than 30g and you don’t activate the ‘leucine ‘ switch. Google Gabrielle Lyon if you are unfamiliar with that term. That’s all there is to it! Eat more meat and see what I mean.
These are my sources for 0.24 g/kg for most people and 0.4 g/kg for exceptional people:
https://sigmanutrition.com/protein-faq/
https://sigmanutrition.com/episode118/
https://medium.com/@dannylennon/researchers-point-to-the-optimal-protein-dose-timing-distribution-to-maximize-muscle-e95c0ab570b0
They don’t say but I suspect that the studies were conducted based on 3 meals per day since that’s how the population eats by default. The 0.24 g/kg fits with what previous studies have found per day and we have lots of examples of people who follow the USRDA and aren’t wasting away. Jason Fung’s seems to indicate the classic USRDA is sufficient. A starvation study was conducted that showed 32g-46g day was required to prevent lean mass loss (over what baseline I don’t know – “ideal body weight”)
I am familiar with Donald Layman and Layne Norton’s work on leucine. I think their numbers are high (Layman says 30g protein/meal, Norton says 3-4 grams leucine) because Layman’s studies are based on elderly (70’s) subjects showing anabolic resistance and Norton works in bodybuilding where you’re breaking down your muscles with hours of high-volume lifting. If you don’t want to be big – I want to maintain myself at a reasonably lean 70kg and be reasonably strong for my weight – and you’re not old, I think the classic USRDA is reasonable.
If excess protein doesn’t reduce longevity then it doesn’t matter really – e.g. double your required protein doesn’t harm you short term.
Hi Bruce, thanks for posting your sources very interesting, I’m going through them now. BTW, re Sigma Nutrition: I recently listened to a solo podcast Danny did on protein where he states 2g protein/ kg bodyweight/ day is the optimum to go for for most adults: same as Chris Masterjohn and several others. Dr Stuart Phillips is slightly less at 1.6g-1.8g, Dr Lyon, Dr Layman, Dr Naiman, all more than that – with Dr Baker and Dr Antonio and Martin Berkhan (creator of 16/8 intermittent fasting) at much more than that. Then you have Ron Rosedale, Dr Mercola, Dave Asprey & Valter Longo on the other side. They claim that by spiking M-Tor even intermittently this will increase your chance of cancer – but I’ve never seen any convincing evidence for this as long as the Mtor is spiked acutely as opposed to chronically. . I’ve listened to both sides in great depth and know which side I fall on.. If you do find any convincing evidence to support Rosedale/ Longo/ Asprey/ Mercola do let me know as I have been looking for a long time but found nothing – as of yet anyway..
Re the articles you linked to, I think the confusion re the 0.24g/ meal is that whilst she just refers to ‘protein’: I think she is actually means fast proteins such as whey. Meat will slowly be digested over many hours, which is why Shawn Baker, Berkhan, Luis Villanour (ketogains) and others can make such gains on only 1 or 2 meals/ day. If they could only absorb 0.24g from their 1 or 2 meals/ day then their workout regimes would have crushed them after a few weeks. I agree though that 50g of whey may be overkill per meal, since it is too fast to stick around in the system for long. Nevertheless I believe a bolus of 50g of whey to be very useful just after (or even better, just before before) a fasted HIT resistance training session, a la ketogains. It all depends on context I guess..
Hi Rob,
No, I don’t have any other sources for low protein although Mangan has some references to lower numbers in his article on optimal protein where he mentions slightly over 1g/kg/day for elite bodybuilders.
https://pdmangan.com/the-sweet-spot-for-protein-intake/
There is the (not very scientific) argument that bigger individuals (within a species) don’t live as long and that this applies to humans as well as animals. I don’t know if this is true but I don’t necessarily want to be big as much as maintain an optimal bodyweight for my height/frame with reasonable strength. Think Bruce Lee vs. Arnold Schwarzenneger.
Yes, I agree with you Bruce. I think if you are following a ‘HIT’ approach to weight-training – as recommended by Dr Doug Mcguff (‘Body by Science’), Mike Mentzer, Ted Naiman and others (and as followed by Dennis and myself) then you will never get ‘massive’: particularly when combined with intermittent fasting. However, as Doug says in a recent podcast with Lawrence Neil (excellent podcast on HIT): whilst you will never be mistaken for a bodybuilder whilst fully clothed (too lean), people will be quite surprised to see how well defined your muscles are when you are on the beach.. So yes, definitely Bruce Lee as opposed to Arnie! Have a look at Ted Naiman if you are not familiar with his approach: he has a very ‘Bruce Lee’ like physique achieved purely from daily calisthenics (body weight exercises) coupled with a lot of daily protein. He has no time for the Rosedales of this world or claims that high protein leads to increased risk of cancer..
Mr. Mangan,
“gluconeogenesis is a demand-driven process”
I assume that the demand that typically drives it is energy deficit. Is this correct?
A demand for glucose. Blood glucose levels are defended, so if no carbs are eaten and glycogen stores are next to nothing, gluconeogenesis increases. Ketones are also generated, and these spare glucose.
Sorry to beat this to death – just curious how it works.
So I wonder if someone like Ted Naiman is, by eating large amounts of protein (say 80 grams/meal twice a day), getting the safe effect as if he replaced some of his protein with relative low insulinogenic starchy foods. I assume the protein he eats that isn’t used for muscle protein synthesis would undergo gluconeogenesis since there’s very little glucose produced by his diet due to lack of carbs.
The excess protein drives insulin, is turned to glucose, etc. So what’s the difference?
Note I say low insulinogenic carbs. Some carbs (oatmeal, pasta, bran, certain types of bread etc.) are approximately the same in terms of insulinogenic properties as meat. Not potatoes though!
I am trying to imagine a smart way to eat carbs for those of us who want to continue eating them. I admire your discipline but cannot match it.
Meat is like firepower – if it’s not working, you’re not using enough!