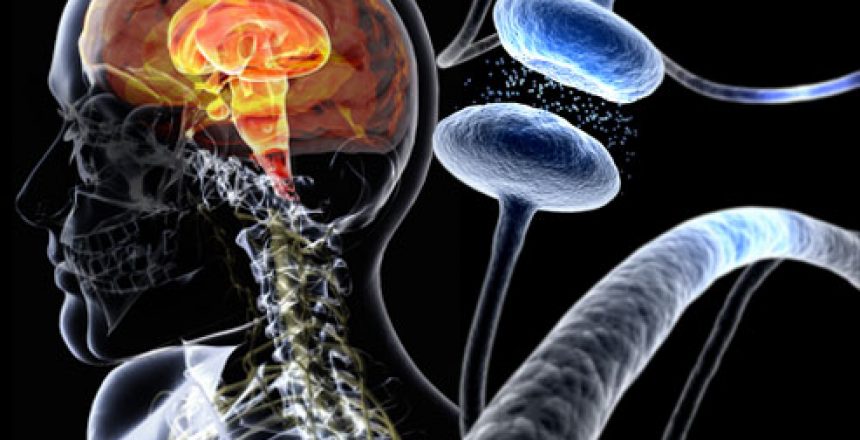
As I wrote about in my book Dumping Iron, excess body iron stores are implicated in many diseases, including heart disease, diabetes, and cancer, as well as in aging itself. Among the other diseases that excess body iron is implicated in are Alzheimer’s and Parkinson’s diseases, which are characterized by (among other things) neuronal cell death. A process that causes cell death has recently been elucidated and this is iron-induced cell death, ferroptosis.
Programmed cell death
Programmed cell death occurs when cells initiate actions that lead to cell suicide, or apoptosis. This is thought to be done as a safety measure that ensures the integrity of the organism. When cells die in a non-programmed way, necrosis occurs, which presents problems for the organism, so cells have ways of killing themselves in the face of certain stimuli.
Programmed cell death is also essential in embryogenesis, tissue homeostasis, and immune response.
Ferroptosis is a newly discovered mechanism of programmed cell death, and as its name makes evident, iron is involved.
Much research has gone into elucidating the specific biochemical reactions that take place in ferroptosis, but for now, I’ll stick to basics. Three different chemical entities are involved in ferroptosis:
- iron
- polyunsaturated fatty acids
- glutathione.
Polyunsaturated fatty acids are necessary components of cell membranes, but they are readily oxidized. Free iron, that is, iron that is not bound by proteins such as ferritin or transferrin, react with the polyunsaturated components of the cell membranes to form highly toxic lipid peroxides.
Glutathione, the cell’s most important and abundant internal antioxidant, is used to detoxify these lipid peroxides. If enough glutathione is not present, then lipid peroxides accumulate to critical levels, at which point the cell executes its cell death program, ferroptosis. Schematic illustration, below. (Source.)

Cystine, the dimerized form of the conditionally essential amino acid cysteine, enters the cell to be used in the production of glutathione. When it’s blocked, or when enough isn’t available, glutathione decreases, lipid peroxides cannot be detoxified and therefore accumulate, at which point ferroptosis occurs.
There are a few important points here as this process relates to health – this isn’t just a bunch of dry biochemistry, and in any case, I’ve greatly simplified it.
Iron chelators – molecules that bind and remove iron – prevent ferroptosis. This is important because it shows that free and not bound iron initiates the process. If the iron were bound – to ferritin, transferrin, hemoglobin, or any of a number of other iron containing molecules – iron chelators would be powerless to stop it.
Adding iron to the cell culture medium increases ferroptosis. Again, free iron is the cuplrit
Autophagy, specifically ferritinophagy, the breakdown of ferritin, is required for ferroptosis. That’s where the free iron comes from, the breakdown of ferritin.
Polyunsaturated fatty acids in cell membranes come from the diet. The membrane phospholipids that become peroxidized are composed of arachidonic acid, which is made from dietary linoleic acid, the most abundant fatty acid in seed oils. Since polyunsaturated fatty acids (PUFAs) compete for enzymatic conversion and subsequent space in cell membranes, excessive consumption of seed oils means a greater fraction of peroxide-capable arachidonic acid compounds in the cell membrane. Thus, diet can be linked to ferroptosis. One study says that the lipid peroxidation is specific for two omega-6 fatty acids only, arachidonic and adrenyl derivatives.
Lack of glutathione is also critical in ferroptosis, and this can also be linked to diet. Cysteine, the rate-limiting amino acid in glutathione synthesis, is found in all protein-containing foods; whey protein is especially abundant in cysteine. Diabetics and others suffering from oxidative stress have low levels of glutathione, and it’s said that aging could be (in part) a cysteine deficiency syndrome.
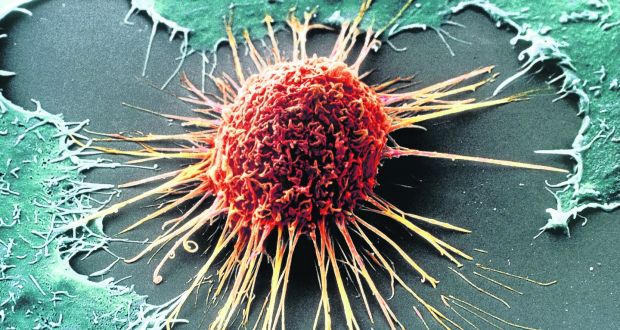
It appears that the high iron content of cancer cells can be exploited by making them enter ferroptosis, for example with the drug artemisinin or with vitamin C.
The process of ferroptosis provides another mechanism by which excess body iron, polyunsaturated fats in seed oils, and the absence of sufficient protein, can harm health.
Excess body iron in the form of high ferritin means that abundant ferritin is available to be broken down via ferritinophagy, leading to free iron inside cells. As I wrote in my book, ferritin is like stored dynamite: in theory, it’s safe, but you don’t want a bunch of it lying around your house. The more you have, the more likely an accident can happen.
Consumption of seed oils leads to a high proportion of the kind of membrane lipids that lead to ferroptosis.
Low dietary protein, or oxidative stress brought on by diabetes or other conditions, leads to low glutathione, which promotes ferroptosis.








16 Comments
Excellent post implicating potential ferroptosis in pregnancies from irrational iron supplementation causing toxic iron overload, a possible factor in embryonic damage in the first trimester of pregnancies leading to phocomelia or limb deformations in fetuses.
Should I be routinely donating blood to reduce iron stores and if so how often
Hi Mark – I covered all of that in my book, Dumping Iron.
I’ve been donating blood every 2-3 months for the past year. I discovered back then that my serum ferritin was around 450, so way too high. I’ve been able to bring it down to around 160 since then, but I still have a little ways to go before I am where I want to be (100 or lower). After that I still plan to donate blood to keep it at that level, but hopefully less often.
Rob, did you mean to say that you are down to a ferritin count of 160? If so, at the rate that you’ve been going since beginning at 450, you’ll be under your target with the next blood donation….
Thanks for the reply, bigmyc – you were right on the mark. I just got my ferritin tested this week, and it’s now down to 60, which is right where I need to be. I was surprised it had dropped this much in one year, but the 5-6 blood donations did the trick. Now I need to keep it under 100……..would you suggest 1-2 donations per year would be adequate to do that? PD, your input would be very much appreciated also.
Hi Rob – yes, 1-2 donations a year will keep an already normal ferritin in the normal range, below 100.
RB Lauffer in Iron and your heart, 1993, page 244 shows a table of iron donations to get ferritin to 41-62 starting at “over 282” requiring 11 donations at prescribed intervals.. Starting at 160, it would take 2 more donations to get to 100 and about 5 more to an optimal 40-50 ng/ ml ferritin range. The author reduced his level from 88 to 33 with 2 and to 11 with 3 donations (page 246). My latest ferritin was 36 on a largely vegan plus fish diet including phytate rich foods with no blood donations.
Hi P.D.
What do you think about cooking in carbon steel or cast iron cookware?
I’ve read somewhere that they leak iron, especially with acidic foods but also with non-acidic.
Thank you
Hi Marco, yes, you get some iron from cast iron cookware, especially with acidic foods like tomato sauce. Whether you should care is another matter. If you really need to watch iron levels, then use another type of pan; if you’re iron is good or you’re on a decent iron-lowering program, it probably doesn’t matter a lot. It gives you a mg or 2 of iron per meal.
Valuable knowledge, that. Have to re-read the middle para’s when I’m more awake.
(off-topic)
Mr. Mangan, have you looked into ginger?
It looks quite promising to me.
Ginger is overrated. Mary Ann is better.
If after several blood donations, someone gets their ferritin to a low number like 10 or 20, could that person still have high levels of free iron? If yes, how would you then get rid of it if losing blood and having a low ferritin number doesn’t do the job?
While someone with that low of a ferritin value could have some iron dysregulation and hence a certain amount of free iron, it seems unlikely that it would be much. However, if interested in mopping up free iron, chelators such as IP6 or curcumin can be of value.
Free ionic iron is toxic and is not in present blood: all is bound in some way to keep iron requiring pathogens from multiplying in normal blood. Most of the iron is firmly tied up in hemoglobin, some inside storage protein ferritin as a compact ferric iron phosphate core that releases iron as soluble ferrous ion as needed and as transferrin, another iron storage protein measured as serum iron or partly filled or unsaturated iron binding capacity or UIBC plus maximum or total iron binding capacity (TIBC). Normal ratio of serum iron/TIBC is 20-50% saturation with over 50-60% is seen in hemochromatosis from often huge genetic iron overloads, sometimes visible as dark skin spots of hemosiderin from irreversibly deposited degraded ferritin Best to measure all iron proteins in the hematology panel: Hb, ferritin, serum iron (UIBC) and TIBC, etc