Before the 20th century, coronary heart disease was all but unknown, but starting in the 1920s, the rate of heart disease rose significantly. By mid-century, the rate of heart disease was alarmingly high, and by 1970, it’s declined significantly. What caused the rise and subsequent decline of heart attacks?
Rise and Fall of Heart Attacks
Dr. David Grimes wrote: “Few people are aware that coronary heart disease (CHD) has been an epidemic of the latter half of the 20th century. It is now almost over.”
He put together the following chart showing the rise and fall of deaths from coronary heart disease. As can be seen, heart disease deaths were nil in 1910, rose to a peak about 1970, and have declined dramatically since then.

It’s important to note that these are age-standardized rates, which compare different populations after adjusting for age. Absolute (crude) mortality rates are still high, but this is more of a function of the older age of our current population.
I sought statistics that would corroborate Dr. Grimes’ numbers, and found some: Decline in Cardiovascular Mortality (2017), published in the journal Circulation Research. The article contains the following chart, and the numbers are similar to those reported by Grimes.
Deaths from cardiovascular disease in men only have fallen massively.
Here’s a graph showing the rise and fall of heart disease deaths from 1900 to 2010. (Source.) These statistics are not age-adjusted.

What factors are responsible for the rise and subsequent decline of heart disease? What factors are not responsible?
Three Factors: Cigarettes, Hydrogenated Seed Oils, and Sugar
To see what factors may have caused the rise in heart disease, we should ask what factors were low to non-existent in 1900, and that are known to cause heart disease, which then increased in the course of the century.
Cigarettes
One such factor is cigarettes.
Annual per capita cigarette consumption in the U.S. in 1900 was 54 cigarettes. (Source.) Machine-manufacturing caused the price of cigarettes to drop, and per capita consumption rose dramatically to over 4000 by 1965, and currently stands at about 1000. Less than 5% of Americans smoked cigarettes in 1900, while 42% were smokers in 1965. (Source.)
Cigarettes are a well-known cause of heart disease.
People have of course been smoking or otherwise using tobacco for hundreds of years in the Western world. But cigarettes are a uniquely damaging form of tobacco use, because their smoke is inhaled into the lungs.
Most pipe and cigar smokers do not inhale, so they have a lower risk of causing heart disease, and smokeless tobacco produces no combustion products.
The culprit is not nicotine, but the chemical stew of thousands of toxic chemicals that forms when tobacco is ignited.
Hence, cigarettes are a prime factor in the rise of heart disease. Since cigarette consumption has declined dramatically since the peak of the heart disease epidemic, that’s further evidence that they caused the heart disease epidemic.
Hydrogenated Seed Oils
Hydrogenation is the process of chemically modifying unsaturated fats to make them saturated. Margarine and shortening are made this way.
In this process, artificial fats, called trans fats, foreign to human physiology are created.
Crisco, the first shortening made from vegetable (seed) oil, was introduced in 1911.
While coronary heart disease had been noted at autopsy in the 18th and 19th centuries, it was not until the 20th century that heart attacks could be diagnosed in the living. It was in 1912 that the first diagnosis of a heart attack in a living person was made.
By the 1920s, the coronary heart disease epidemic had begun. The passage below is from Dr. David Grimes.
The important 1963 review by Dr Maurice Campbell of Guy’s Hospital took data from the Registrar-General’s Statistical Reviews of England and Wales, acknowledging advice from Sir Austin Bradford Hill, and it gives us a great insight into the emergence of CHD. He felt that from 1876 (the earliest public records) until 1921 the death rate from diseases of the heart in general changed very little, and there was no specific mention of CHD. However, the death rate from diseases of the heart started to increase during the years 1922–24 and this would appear to have been the onset of the epidemic. The death rate from CHD in England and Wales increased from 2.9/100 000 in 1921 to 16.6/100 000 in 1931. The recorded deaths from cerebrovascular disease also increased, fewer but by the same factor as CHD. Campbell commented about the increase of CHD deaths after 1921 that ‘the death rate had doubled by 1927, doubled again by 1929, again by 1933, again by 1939, again by 1948, and again for the sixth time by 1956’.
Even mainstream medicine recognizes that trans fats are connected to coronary heart disease.
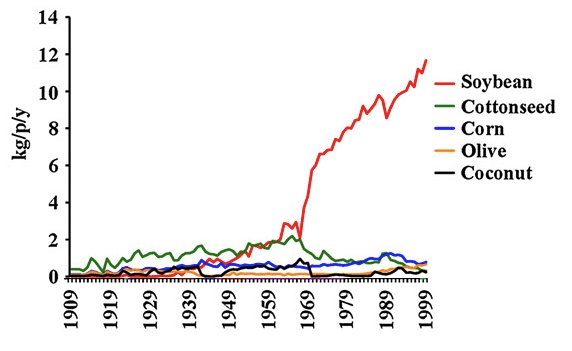
Besides hydrogenated seed oils, regular liquid seed oil use became commonplace in the 20th century. Soybean oil use per capita rose more than 1000-fold from 1900 to 1999. Use of vegetable (seed) oils raises the risk of heart disease.
Sugar
Sugar consumption rose greatly in the 20th century. See chart below.
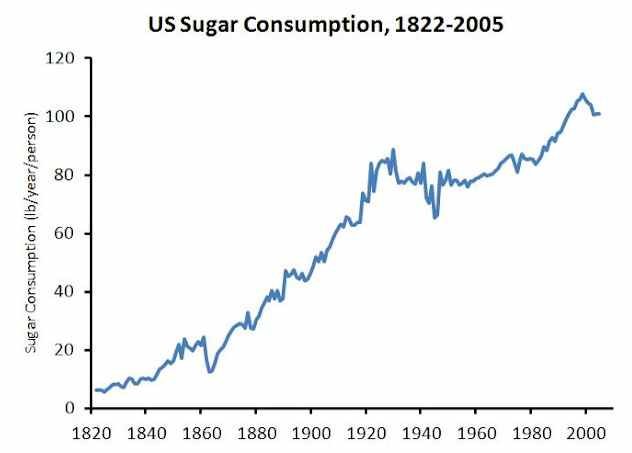
Sugar is associated with coronary heart disease.
The decline of heart disease
We also saw from the above charts that heart disease has greatly declined since about 1970. Most of the decline is due to reduced rates of sudden cardiac death, the classic drop-dead of a heart attack scenario.
The reasons for the decline could be many.
An article on this topic suggests the decline of smoking rates, lower cholesterol levels, as well as better prevention, such as statins and aspirin. I’d add use of fish oil, and more health consciousness, including regular exercise.
Smoking rates are clearly a major factor.
Heart attack rates were declining before statins came on the scene.
However, aspirin use against heart disease has been known since around 1940, so that might be a factor. Widespread use of aspirin to protect against heart attacks began in the 1980s.
Conclusion
Deaths from coronary heart disease rose and declined dramatically in the 20th century.
My candidates for the cause of its rise are cigarettes, seed oils, and sugar.
Meat didn’t have anything to do with it.
The heart disease epidemic of the 20th century shortened the lives of millions, particularly men.







44 Comments
This well-intentioned is misleading. It is also partially based on an outdated paradigm that favors a pharmaceutical model of intervention for CVD. While it is a fact that deaths from CVD have declined, the rate of heart disease has not declined. To title the article, “The rise and fall of heart disease” is therefore not factual. Perhaps our management of CVD has improved (quality of life issues notwithstanding). Table 44 of the CDC report, “Respondent-reported prevalence of heart disease, cancer, and stroke among adult aged 18 and over…” for the years 1997 through 2012 shows no improvement in the rate of heart disease, with the percent of the population varying from 11.3 to 11.8%.
Regarding causation, references to cholesterol management are 1960s medicine at its finest. While statin drugs have been prescribed for 30 years, to suggest that thee drugs deserve the credit for a decrease in cardiac deaths is misguided. As stated above, better management of CVD to prevent death does not translate into lower rates of CVD. The fact that after spending hundreds of billions of dollars on statin medication has not decreased the rate of disease is typical of the cognitive dissonance surrounding this topic. It has been 30 years, of lower and lower levels of cholesterol that have not reduced the rate of CVD. The burden of proof of the effectiveness of lowering cholesterol and prescribing statins remains squarely on the shoulders of those that promote this falsely held position. Stated more clearly, when the facts do not match the theory, it is not the facts that are wrong.
I don’t see where I said statins or cholesterol management are responsible and in fact don’t believe they are. Perhaps you could read more carefully.
You referenced an article, “…suggests the decline of smoking rates, lower cholesterol levels, as well as better prevention…” It is understood that the most common intervention to accomplish the lowering of cholesterol is Statins.
I was referencing someone else. That’s not my opinion. I wrote, “Heart attack rates were declining before statins came on the scene.”
You’re new here, right?
This is the first time responding to an article. Having been engaged in integrative medicine for 40 years it was my opinion that this general assertion that CVD was dead was misleading. What is the relevance of your asking if I am new here?
The reason I asked whether you were new here is because I’ve written extensively on how the diet-cholesterol-heart theory is BS. Cholesterol doesn’t cause CVD.
As regards “this general assertion that CVD is dead”, it’s about age-standardized rates, which I emphasized, and furthermore I cited several peer-reviewed papers that agree this trend is happening. If you don’t want to believe it, that’s your prerogative.
No offense was intended. I asked because I thought there may be a legitimate reason you asked if I was new. From your response I see that your reason to question was related to our discussion. I am not familiar with your work or prior writing.
As a few engaged in this dis ussion have stated, including me, your conclusions that heart disease is dead cannot be substantiated in the literature without manicuring the variables to fit that paradigm. My willingness es to not agree with your assesmrnt is not personal, it is not an attack of your credibility, and certainly not based on my awareness of your prior positions. If offense was taken please accept my apology for misrepresenting my objective: to disagree with your interpretation of the leading cause of death as a former area of concern.
Thanks, Tom, no offense taken. The heart disease question is of great interest to me, since I was young when it was at its peak. My father started suffering angina pectoris at age 49, and though heart disease didn’t kill him, he lived with it the rest of his life and I know it put a huge damper on his outlook. I suppose the knowledge that you could have a heart attack at any time would do that. I was determined that it would never happen to me.
I share your concerns as I have a family history of CVD. The entire paradigm of vascular disease is shifting. A study lat week demonstrated that of the women that sustained an MI, 25% had totally clean arteries! The current thinking is that the micro circulation compromise that occurs to tiny vessels that feed the heart are compromised by elevated glucose levels, causing a decrease in micro circulation.
In African American patients I have personally reduced gangrenous lower extremities patients scheduled forBK amputation with a low carbohydrate diet supported by supplements. I have had high sympathetic types that reversed CVD with a plant based, low protein, high fat diet. There is no cook book approach that fits everyone. Few interventions beat a good history that should include questioning genetic predisposition.
I wish you good health. There are few physicians that have not become victims of today’s medical education that is dominated by symptom management through drugs. There is no such thing as a beta blocker deficiency. Your initiative and willingness to take responsibility for your health will serve you more than allopathic medicine can provide. Be well.
You’re being overly aggressive with Thomas. His note was conversational and a helpful addition to the post you wrote. Both of your responses could’ve been toned down and more engaging. Less blocking and tackling.
Interesting post, but I think you need to be careful with the conclusions you reach from the data presented. The data you present do suggest that deaths from coronary heart disease have declined since the 70s (age-adjusted). The data don’t show that coronary heart disease has actually declined since the 70s, unless I missed something. It may be that coronary heart disease is still just as prevalent now as back then, but something is preventing people from dying from CHD until they reach a much older age. Also, with sugar consumption and soybean oil consumption both still increasing up until the present time, it doesn’t make sense that rates of CHD would be declining so rapidly (if we assume that sugar and industrial seed oils have something to do with CHD, as I believe they do). I’m just speculating here, but maybe the decline in smoking since the 70s is largely responsible for the apparent decline in mortality from CHD since then. In other words, back in the 70s, when smoking rates were very high, perhaps folks with CHD were more likely to die suddenly from it (and at a younger age)……..whereas now, folks with CHD (who do not smoke) are able to linger on for quite a few years with it, and survive until a much older age before succuming to CHD or something else. Hard to say without looking into this much further. I do not think statins are responsible for the apparent decline in mortality due to CHD, as the vast majority of studies I’ve seen show that statin use may lower cholesterol, but it does nothing to lower a persons risk of dying from CHD.
While I agree with everything here, another factor that Dr. Kendrick has pointed out is the elimination of lead in gasoline. Lead is apparently a very potent cause of damage to the endothelium and its rise and elimination correlates well with heart issues. I highly recommend his ongoing series on What Causes Heart Disease. It is not only a wealth of information but a great study on how to think about problems like CVD.
Yes I agree with you. Dr Kendrick is now up to Blog post 50 discussing with reference to the evidence, the causes of CVD.
From the charts it would seem that smoking cessation is playing a major role. I was all ready to denounce sugars but the chart seems to exonerate them.
Also, the incidence of cancer mortality rates has been on an upswing, so perhaps just a higher percentage of people are now dying of cancer, and therefore fewer are dying of heart disease.
OT – but regarding your exchange with Ted Naiman on twitter regarding the carbohydrate-insulin model (I do not have a twitter account so I am commenting here):
Ted said that: “the carbohydrate-insulin model is completely dead, because protein is insulinogenic and yet if you eat nothing but protein you will be lean AF.”
However, IIRC you have said that protein glycogenesis appears to be demand-driven in contrast to supply-driven carbohydrate glycogenesis. If so, then I see no paradox. The more carbs (especially refined and simple carbs) you eat, the more glycogen is produced and the more your insulin rises. In contrast, even if you eat excess protein, your body only converts to glycogen that which it needs. Is that the case?
Gluconeogenesis is the process that makes glucose from protein, and in turn glucose could be made into glycogen if necessary. And it is true that GNG is demand-driven, not supply-driven. Excess protein doesn’t “turn into” glucose. That said, I’m not sure what to make of Ted Naiman’s statement – and he could be right of course.
My thinking: when you ingest protein, it raises insulin to a level high enough to stimulate muscle protein synthesis. If you ingest carbs with that protein, it raises insulin a lot more, but that insulin does not further increase muscle protein synthesis. If you ingest lots of protein, maybe insulin doesn’t go high enough to induce obesity.
It also occurred to me that the reason for “rabbit starvation” is production of excess ammonia – not sure if that’s the case, but if it led to that, it would certainly lead to sickness and death regardless of what insulin does.
This is a rather interesting self experiment by one of my associates Eli ( all of us in our practice do rather extreme health self experiments on a regular basis). Over the past several months he eats nothing but one and a half pounds of ribeye steak daily, which he consumes in one serving.He has lost several pounds doing this, though he was slim to begin with , and here are his very recent labs:
Insulin 1.0
IGF-1 124
Triglycerides 66
Glucose 80 ( up from 65)
HDL 88 ( up from 85)
T cholesterol 525
LDL 350
So on nothing but red meat his insulin and IGF-1 are very low and his Trig/HDL are also very good. I’m not sure what to make exactly of his other numbers and at this point I’m not sure that anyone would know with any certainty.
Thanks for the reply.
I had formerly thought that excess protein did “turn into” glucose, and was happy to find out that it was demand-driven, which resolved the paradox IMO. The simple/refined carbohydrate-insulin model is not the *only* insulin model, but it definitely appears to still be the most important one with regards to obesity and disease.
Protein also raises glucagon much more than carbs, so it is not an apples to apples comparison. Also, I think Ted’s point is a bit irrelevant (whatever his point is) since chronically elevated insulin seems to be a likely causative factor in almost every major disease state (diabetes, cancer, dementia to name a few) and it appears to prevent weight loss, so lowering insulin is essential for most people. Also, as Dr. Fung, Paul Jaminet and others have stressed, there are at least 8 different pathways that promote obesity, and insulin is just one of those.
This discussion has evolved in an interesting manner. Many of the issues raised require greater attention than can be provided here. For example, GNG is an individual phenomenon with a strong genetic component. Demographic data and direct lab work sponsored by te Federal government has revealed that Northern Europeans have the greatest propensity to tolerate high carbohydrate diets, with native Americans having the leasttolerance for carbohydrate. The rates of type II diabetes and CVD amount native Americans is well known. Subsequently, this group also has been demonstrated to have higher rates of GNG, whereras the Northern Europeans had the lowest rates of GNG. Though someone that has eaten one steak a day and produced beneficial blood work is not of value in forming conclusions about this topic, other than to suggest that it works for him. Obviously one meal per day that this person consumed enabled him to benefit from the effects of intermittent fasting. He was also slim to begin with, suggesting good blood sugar predisposition.
From a health/well-being perspective, protein consumption should vary based on gentics and autonomic characterization. High sympathetic types do better with less protein. High parasympathetic types do better with more protein. There are gradients in between these extremes.
Our current model of medicine is a vertical model: one disease =one cure. It would be great if it was that simple. While Big Pharma has coopted the intervention/educational process and reduced it to symptom management not restoring health, it is important that we not become victim to that model
Some very interesting thoughts there. It is certainly no surprise that protein diets are more tolerated in certain areas of the world, while carbohydrates are tolerated in other areas, probably based on the eating habits of specific ancestral groups which almost certainly were quite variable.
I had never heard of the distinction between sympathetic and parasympathetic tone and protein tolerance. That’s very interesting. Of course it is possible to intervene in this regard. For example, one can tone down sympathetic tone via exercise and also with the use of beta blockers. Exposure to heat also will decrease sympathetic tone rather dramatically. https://www.jstage.jst.go.jp/article/biomedres/36/2/36_135/_pdf
I wonder if you make such an intervention if you are then better off increasing your protein intake?
As for Eli and his all meat diet, I’m not certain that it is working for him. I am not at all in the camp of the mainstream medical community when it comes to cholesterol, but I don’t know that I would want his rather extreme values either. Also keep in mind that an all protein diet is very significantly elevating mTOR. Never a good thing after the age of 20.
Some great comments here, love the way this discussion is developing (you have an extremely educated audience Dennis!) Paul, whilst I agree with most of your comments I have to disagree with your point re MTOR. My view is that Eli’s underlying MTOR levels must be significantly lower, since he is only eating once a day and fasting for the remaining 23 hours. Yes, he will significantly spike MTOR when he eats his meat feast, but this is what we all need: infrequent daily spikes in MTOR to promote growth, vitality etc set against the backdrop of low chronic levels of MTOR. Couple this with some of the research presented by Ted Naiman and Shawn Baker that protein does not increase systemic levels of MTOR: only chronic carb consumption does that. Protein causes muscle-specifc rises in MTOR which can only be a good thing if you are incorporating some element of resistance training into your weekly schedule – as I hope everyone reading this already is.
Moreover, the reason for the difference in terms of insulin being linked to fat gain over the different macros is also partly explained if we remember not to be fooled into looking at insulin in isolation – a common mistake I see many people make. Protein (particularly BCAAs) massively raise insulin, yet the accompanying rise in glucagon cancels out much of the deleterious effect otherwise it would also cause massive hypoglycaemia amongst other tings – which is not observed in practice. Carbs however increase insulin and lower glucagon, whereas fat only increases glucagon without affecting insulin. That’s the danger I often find of looking at various factors in isolation without accounting for the wider systemic effects.. What does everyone else think of MTOR? If anyone is of the view that keeping it chronically low as opposed to spiking it daily is a good thing, could you link through to studies backing that up (I haven’t seen any!) Fantastic discussion guys!
And just one other point: from looking at Eli’s bloods I can see that his underlying level of IGF-1 is very low so that to me would be a good indicator that his MTOR is NOT being chronically activated, since the 2 are frequently correlated. Also, whilst his blood glucose has gone up: in the face of very low insulin I think this is becoming more widely accepted as being a moot point. After all, if the raised blood glucose were deleterious then the body could easily raise insulin to remedy the problem – but it chooses not to do so. As per my point above, context is king: raised glucose + raised fasting insulin = bad news but raised glucose + low fasting insulin = no worries as far as I am concerned (unless your are a Type 1 diabetic of course!) As per Dennis’s recent post, the blood markers which tell you all you need to know are the Trigs/HDL ratio and fasting insulin. If they are good, I would say that blood glucose elevations and elevations in LDL are irrelevant. Other key marker of course is waist circumference to height ratio (as well waist circumference changes relative to weight changes) : I bet Eli’s has improved indicating improved body composition – which will no doubt lead to health improvements for him?
Rob, you make many great points.
I agree that glucose in the presence of low insulin is moot. That is not the same animal as diabetes, but is often mistaken as such. In fact, even in those with metabolic syndrome, up to 50% will have coronary calcium scores of zero.
Since mTOR is such a sensitive cellular energy sensor, and is ubiquitous, I’m sceptical that such a basic growth promoter as amino acids would be muscle specific in their mTOR activation.
I prefer rapamycin to fasting because I know it’s half life and so I feel that it’s more controlled. I like to inhibit mTOR about 20% for a couple of days and then have it totally restored, whereas with fasting it’s inhibited daily and I worry that mTOR 2 May be affected.
Excellent point correlating IGF-1 with mTOR and I feel that it may be our best biomarker at present. I think a good range is 100-150.
I agree that the triglycerides/ hdl is our best predictor, but I’m not yet willing to totally disregard very high ldl levels.
I recently came across this paper (https://www.sciencedirect.com/science/article/pii/S1359644616301921) which discusses what the author believes to initiate coronary artery disease. He states that “uncontrolled cell proliferation in tunica intima of human coronary arteries is the initiation of the coronary atherosclerosis.”
That sounds like mTOR and/or insulin could be doing it, and would explain why aging is a risk factor for CAD.
That’s a great article and very much confirms the Blagosklonny argument that age- related diseases start with uncontrollable proliferation of dysfunctional senescent cells. This would be true not just of CAD, but all diseases of aging.
That article was a great find.
In my mind mTOR inhibition is now a no brainer, but I’m also wondering if it should be coupled with senolytics as well like tocotrienols and quercetin.
Totally agree Paul – I have been liberally adding capers to my lunch and dinner for quite a while now (according to Wikipedia they are the food source which contains the most quercetin. I always prefer the wholefoods route – where one exists!)
Hi Paul – very interesting observations. Yes, you bring up the important distinction between mTOR 1 & 2. I wish I could remember where I read it, but one of the well-known protein researchers was making the point that as long as an individual is ‘priming the pump’ by undertaking regular resistant exercise, then increases in mTOR associated with amino acids primarily affect muscle hypertrophy as opposed to raising systemic levels of mTOR. Apologies I don’t have the reference, but it was either Dom D’Agostino, Ben Bikman, Ted Naiman, Stuart Philips, Gabrielle Lyon or Shawn Baker. I would highly recommend everyone to seek out podcasts featuring these individuals – very instructive. The last 5 in particular strongly advocate the health & performance benefits of a high protein/ high fat/ very low carb approach. They maintain that ketosis can still be just about be maintained even in the presence of high protein intake because gluco-neogenesis is essentially a ‘demand-driven’ as opposed to a ‘supply-driven process’ – ie no surprise that the body uses homeostatic mechanisms to only produce as much glucose as it strictly requires for essential processes and no more. Plus the direct insulinogenic effect of the amino aids are negated by the corresponding increase in glucagon they stimulate.
There really does appear to be something in Shawn Baker’s ‘zero carb/ carnivorous’ diet approach – if you listen to his podcast there are many people who like him have drastically increased both their health & performance markers by even moving from a full-on keto approach to then follow his approach. The science has yet to get to grips with this, but I am sure in time it will. He does explain somewhere why increased LDL is perfectly expected and benign following his approach, so I have to say that aspect does not worry me any more in the face of low fasting insulin. I would just recommend everyone out there to listen to these podcasts – there is a lot more information out there than you imagine and it is growing every day. (Still not enough to shake me out of my low-carb/ high protein/ moderate fat paradigm though – yet – but if I had a significant health challenge as these guys did – then I would definitely experiment with it for a month or two!)
Hi Paul,
Just one other thing to add: I was seeking out the links for you explaining why very high LDL levels seem to be entirely inconsequential as long as HDL is high and triglycerides are low. The guy who has written about this the most is Dave Feldman, for example see his podcast appearance here: https://lowcarbcardiologist.com/lccp036-dave-feldman-challenges-everything-we-think-we-know-about-ldl-cholesterol/#.W03svS3MwdU Another cardiologist (Dr Nadir Ali) also explains it very eloquently on a new podcast today on Ben Pakulski’s podcast. So, I would argue that yes there is enough evidence out there now to disregard very high LDL levels – but it is cutting edge stuff so you have to go and seek out the information. But your patients will thank you for it! Dennis – surely this is prime ‘rogue health’ material which you can sink your teeth into?!
Thanks, Rob, indeed it is.
This continues to be an interesting discussion. All ldl particles are not created equally. We’ve known for some time now that the small and dense variety does more harm than the larger and fluffiest types. We have recently learned that the propensity for certain ldl particles to aggregate makes them particularly dangerous. It can be difficult to know these particulars in any given individual, but I’d be concerned that a very high ldl may contain a fair number of the harmful varieties. But I don’t know this for sure.https://www.cardiovascularbusiness.com/topics/lipids-metabolic/ldl-aggregation-marker-cardiovascular-riskhttps://www.cardiovascularbusiness.com/topics/lipids-metabolic/ldl-aggregation-marker-cardiovascular-risk
Hi Paul, yes that was precisely my view too before I began to dig into it a little deeper by listening to the podcasts of Dave Feldman and Dr Nadir Ali – also Ivor Cummings. In fact there are several interviews covering this issue on the ‘Low Carb Cardiologist’ podcast. They believe that there is less of an issue with dangerous aggregation of LDL particles in the presence of high HDL and particularly low Trigs, but inversely a high risk if you have high Trigs and your HDL is too low. To be honest, I am still trying to get my head round it, but please do check out those podcasts for an interesting new perspective – I’m just waiting for the Rogue Health article covering this subject!
Rob H,
Wow. The degree of integration presented in those last two post was the most complete presentation I have seen in along time. Conceptualization skills at that level are rare. The challenge here is conveying such in depth analysis to allopathic medicine and then to patients. My experience is that the overwhelming majority will not desire the responsibility required to make such ab adjustment. Example:
I once had a civil but lively conversation with an ER attending regarding statin use. After 45 minutes of refuting every position she took, especially when explaining the difference between relative risk and absolute risk, her final position was, “At least I feel I am doing something.”
(Off-topic)
I’m just dropping by reporting an interesting/amusing finding:
“Diet quality and the attractiveness of male body odor”
“…dietary data revealed that fat, meat, egg and tofu intake was associated with more pleasant smelling sweat, and greater carbohydrate intake with stronger smelling less pleasant sweat. ”
Source:
https://www.ehbonline.org/article/S1090-5138(16)30193-3/fulltext
“The skin spectrophotometry measure (CIELab b*), indicative of greater fruit and vegetable intake, was significantly associated with more pleasant smelling sweat (with more floral, fruity, sweet and medicinal qualities), independent of sweat intensivt”
Somewhat related…
Despite all the debate among various nutritional camps, all seem to agree that trans-fats are bad for the heart, contributing to atherosclerosis and cardiovascular events.
A couple years ago I tried to find U.S. 20th century per capita consumption rates of trans-fats over time, and had no luck at all.
Surely the data are out there somewhere…
-Steve
Not exactly what you’re looking for but butter vs. margarine consumption might get you close enough.
https://www.economist.com/graphic-detail/2017/04/17/margarine-sales-investors-cant-believe-theyre-not-better
What’s funny – not funny haha, funny strange – is that they convinced us to replace saturated fat with trans fat – CSPI notably did this.
Yes, Michael Jacobson of CSPI was forever pushing trans fats and attacking – among dozens of other healthy foods – saturated fats. I used to receive the publication and slowly but surely realized the utter lies (thank you, Weston A. Price Foundation). As for cigarettes, with all their benefits, Freud’s nephew Edward Bernays really shoved them down the throats of the gullible and easily duped Americans (Torches of Freedom, etc…)
I was having this conversation a few months ago with my brother. We are both in our 60s and remarked how kids’ fathers dying of heart attacks when we were growing up in the 60s and 70s was not uncommon, but it seems pretty uncommon now. We both thought smoking had a lot to do with it.
PD Mangan,
It seems that a few years ago people were talking about excess omega-6 relative to omega 3 as a culprit. Has this been confirmed or discredited?
As far as I’m concerned, that’s very real risk factor, and there’s plenty of evidence to support it, but I don’t think the mainstream discusses it, because it distracts from cholesterol.
Attempting to be brief in regard to this subject is impossible. Introducing a new cause of CVD, Vitamin K2 is understated. Yes, CVD increased when fats were reduced. Making matters worse, when animal fat was consumed it was from grain fed animals. K2 is converted by animals from K1 which is grass/chlorophyll derived.. CVD and osteoporosis began their ascent following this shift from grass fed to grain fed livestock as. K2 levels declined.
The relationship between K2, osteocalcin, and Matrix glad protWINSPIN141ein has been well established. K2 removes calcium from soft tissues, especially arteries, and shuttles calcium into bones. Making matters worse is the advertising and commercialization for the need for calcium to build strong bones and elevated rates of atherosclerosis and osteoporosis , both directly influenced by K2, are the result.
buy instagram hacklink followers.